nuchal thickness should not be measured after 20.6 weeks|nuchal translucent prenatal screening : maker Study Design: Nuchal fold thickness was measured at ultrasonographic examination at 14 to 22 weeks’ gestation without previous knowledge of the fetal karyotype. Nuchal cystic hygromas . Resultados do Euromilhões - 16 de setembro de 2022. O 074.
{plog:ftitle_list}
web4 de jan. de 2024 · If I switch to golf each way betting, I would pay $20 for the bet to cover the wins and places stake, and my payout potential is $54, plus my original $20 stake, giving me a total of $74. That translates to odds of 3.7 compared to .
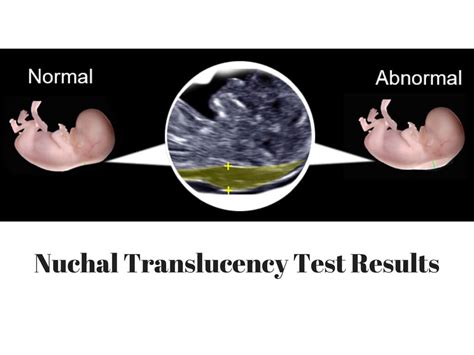
Yesterday we did our 20 week US, and the Dr informed us our LO has a thickened nuchal fold (6.6mm). This is a marker for a chromosonal abnormality, particularly Down Syndrome (T21).Study Design: Nuchal fold thickness was measured at ultrasonographic examination at 14 to 22 weeks’ gestation without previous knowledge of the fetal karyotype. Nuchal cystic hygromas . Had my anatomy scan at 22 weeks and 4 days, and the results just came back. The nuchal fold came back between 6.1 and 7.5mm thick. Under 6 is considered normal. It also . Measurement of nuchal translucency (NT) is an important marker in antenatal screening for Down’s syndrome, trisomy 18 and trisomy 13. Over time, the precision of .
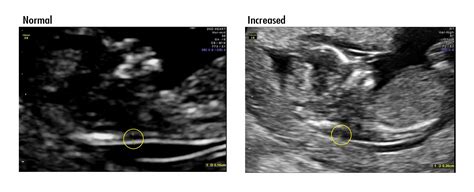
Nuchal translucency is defined as increased if the vertical thickness, measured in the midsagittal section of the fetus, is equal to or greater than 3.0 mm during pregnant .The technique of measurement was tested in a study of 3,338 consecutive pregnancies at 14–21 weeks' gestation. A nuchal-skinfold thickness of 6 mm or greater was identified in 47 fetuses . Methods: A total of 2980 pregnant women for first trimester ultrasonography were routinely offered crown-rump length (CRL) and nuchal translucency (NT) for screening for . The estimated positive and negative likelihood ratios are 53.0 and 0.67 for increased nuchal fold thickness, 22.8 and 0.68 for short humerus, 7.9 and 0.62 for short .
Abstract. Objective To examine the prevalence of all chromosomal defects amongst fetuses with increased nuchal translucency thickness (NT). Methods This is a retrospective . Our data suggest that a nuchal thickness of 2.5 mm might represent a critical threshold for risk stratification. Additionally, the presence of other soft markers and structural . The endometrium should be measured in the long axis or sagittal plane, . <5 mm (although ~50% of those receiving HRT / tamoxifen have been reported to have a thickness of >8 mm 7,13) If a woman is not experiencing bleeding, and the endometrium is thickened, the guidelines are less clear. Either a repeat transvaginal ultrasound or a referral .The NUCHAL THICKNESS (second trimester marker for down syndrome) ️It is measured on an axial section through the head and the level of the thalami, cavum septi pellucidum, and cerebellar.
nuchal translucent prenatal screening
The NUCHAL THICKNESS (second trimester marker for down syndrome) ️It is measured on an axial section through the head and the level of the thalami, cavum septi pellucidum, and cerebellar.
In screening for first-trimester chromosomal abnormalities, measurement of fetal nuchal translucency (NT), evaluation of maternal serum pregnancy-associated plasma protein-A (PAPP-A), and free β . Study Design: Nuchal fold thickness was measured at ultrasonographic examination at 14 to 22 weeks’ gestation without previous knowledge of the fetal karyotype. Nuchal cystic hygromas were excluded from analysis. . Screening for fetal trisomies by maternal age and fetal nuchal translucency thickness at 10 to 14 weeks of gestation. Br J .
The nuchal translucency ultrasound should be done along with the first trimester screening blood work (Down syndrome and trisomy 18) no later than 13 weeks and 6 days. . Good Afternoon all,Finally got my 20 week scan today at 22 weeks 4 days. Everything was measuring exactly on track except for having a thickened nuchal fold. I have booked an . Objective To examine the prevalence of all chromosomal defects amongst fetuses with increased nuchal translucency thickness (NT). Methods This is a retrospective study amongst pregnant women indicated for amniocentesis by nuchal translucency above 3.0 mm and consent to the study. A total of 2,720 cases were recruited during the six-year period from . Studies indicate that women have a heightened chance of getting pregnant with an endometrial thickness of 8 mm to 11 mm in the endometrial thickness chart, which can drastically reduce if the thickness cross 14 mm. The age of an individual also plays a key role in the process. 6. How is endometrial thickness measured? To investigate the performance of nuchal fold thickness, nasal bone hypoplasia, reversed flow in the ductus venosus and tricuspid valve regurgitation in the prediction of fetal aneuploidies in the early second trimester. Methods. This was a prospective study of 870 fetuses at 14 + 0 to 17 + 6 weeks of gestation, performed from 2005 to 2007.
nuchal translucency test results
Transvaginal ultrasonographic cervical lengths were measured 16 to 30 weeks gestation. Primary outcome was cervical length and SPTB less than 35 weeks and the primary exposure variable of interest was cervical length. . Nuchal thickness measurement (15-20 weeks) Footnote2 * Integrity of cranial vault; Examination of brain parenchyma, (e.g .
A targeted sonographic morphological and morphometric evaluation of the umbilical cord was performed in consecutive patients between 7 and 14 weeks of gestation. Crown–rump length and umbilical cord diameter were measured in all cases. Nuchal translucency thickness was measured between 11 and 14 weeks' gestation. Nuchal translucency (NT), measuring the amount of fluid behind the fetal neck in the first trimester of pregnancy, is a crucial indicator for assessing fetal abnormalities in prenatal screening. . revealing fetal NT thickness ≥ 2.5 mm between 11 to 13 +6 gestational weeks. Concurrently, 262 age-matched controls (mean age 28.2 ± 3.8 years .
tensile fatigue testing machine
I keep finding information saying that after 13 weeks 6 days the normal value for nuchal fold thickness is 6 mm . Therefore, could the 5.1mm in my ultrasound be normal ? My previous conversation w/ you . TOP at GA 20 weeks after counseling, no fetal structural: anomaly was noted: TOP, termination of pregnancy; GA, gestational age. . regardless of the CRL or gestational age measured between 11 and 14 weeks. . UK multicenter project on assessment of risk of trisomy 21 by maternal age and fetal nuchal translucency thickness at 10–14 weeks .
Nuchal translucency thickness was measured between 11 and 14 weeks’ gestation. In pregnancies at very early gestational ages (7–10 weeks) an additional scan was performed between 11 and 14 weeks. . to consider incidental the miscarriage that occurred in our case with a single umbilical cord cyst who delivered at 22 weeks after rupture of .In an article published in the American Journal of Obstetrics and Gynecology,Benacerraf and Frigoletto (1987) reported collecting data showing that, regardless of gestational age, nuchal-fold thickness of 303 normal fetuses measured between 1 and 5 mm. Crane and Gray (1991) provided further testing on the measurement of nuchal-skinfold . A fetus with an increased nuchal translucency at 11 to 14 weeks gestation is at risk for aneuploidy, genetic syndromes, structural anomalies, and intrauterine fetal demise in both single and twin .
We then performed an ultrasound scan to determine gestational age from measurement of fetal crown–rump length (CRL), to diagnose any major fetal abnormalities and to measure fetal nuchal translucency (NT) thickness 15-17. In addition, maternal serum PAPP-A and free β-hCG were determined within 10 min of blood collection using automated . There is extensive evidence that effective screening for major chromosomal abnormalities can be provided in the first trimester of pregnancy. Prospective studies in a total of 200,868 pregnancies, including 871 fetuses with trisomy 21, have demonstrated that increased nuchal translucency can identify 76.8% of fetuses with trisomy 21, which represents a false . A positive pregnancy test and plenty of morning sickness are proof enough that you’re pregnant, but your first ultrasound — often around 12 weeks — provides a different kind of evidence that .
nuchal translucency screening
Study Design: Nuchal fold thickness was measured at ultrasonographic examination at 14 to 22 weeks’ gestation without previous knowledge of the fetal karyotype. Nuchal cystic hygromas were excluded from analysis. . 14-22 weeks’ gestation). Mean (±SD) nuchal fold thickness in fetuses with trisomy 21 (4.7 ± 1.6 mm; n = 29) was greater . When the change in the ET during the menstrual cycle is discussed, the ET should be measured several times per woman, as in previous reports. However, these reports included only 23–50 cases, which is not a sufficient number to determine the median ET during the menstrual cycle. In this study, 375 cases were included.
Findings The estimated trisomy-21 risk, from maternal age and fetal nuchal-translucency thickness, was 1 in 300 or higher in 7907 (8 After 14 weeks, a combination of head circumference, biparietal diameter, abdominal circumference, and femur length are measured to come up with a gestational age and/or weight. All women who came to measure NT at 11-14 weeks’ gestation (crown-rump length between 45-84 mm) were considered eligible. We divided patients into 2 groups: women receiving exogenous progesterone and controls. . Nuchal translucency thickness at 11-14 weeks of gestation: French charts and equations [in French] J Gynecol Obstet Biol Reprod . The nuchal thickness also corre- . 19 – 20 4.96 5.11 5.46 5.84 6.20 6.80 6.92. 20 . Both NF thickness and PNT should be dealt with as two separate markers. Although the formation mechanisms .
nuchal translucency measurement
nuchal fold thickness ultrasound
Introduction. Nuchal cord is defined as an umbilical cord that passes 360° around the fetal neck. The prevalence at delivery has been reported as being between 6% and 37% 1-18.Shui and Eastman found the incidence of a single loop to be 20.6%, a double loop 2.5% and a triple loop 0.2% in 1007 infants at delivery 1; however, there are case reports describing a cord .
nuchal fold thickness results
11 de fev. de 2020 · The 5 Whys (or 5 Why, 5W) is a brainstorming technique used in Lean. It was developed by the founder of Toyota - .
nuchal thickness should not be measured after 20.6 weeks|nuchal translucent prenatal screening